Knee Arthritis
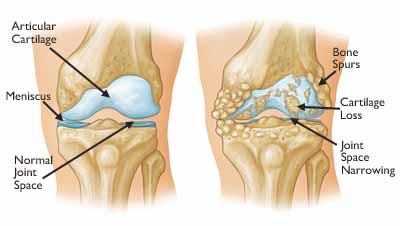
The knee joint is made up of the femur, tibia and patella. The ends of the three bones where they touch are covered with articular cartilage, a smooth, slippery substance that protects and cushions the bones as you bend and straighten your knee. Two wedge-shaped pieces of cartilage called meniscus act as "shock absorbers" between your femur and tibia.
Osteoarthritis
Osteoarthritis is the most common form of arthritis in the knee. It is a degenerative,"wear-and-tear" type of arthritis that occurs most often in people 50 years of age and older, but may occur in younger people, too.
In osteoarthritis, the cartilage in the knee joint gradually wears away. As the cartilage wears away, it becomes frayed and rough, and the protective space between the bones decreases. This can result in bone rubbing on bone, and produce painful bone spurs. Osteoarthritis develops slowly and the pain it causes worsens over time.
Symptoms
A knee joint affected by arthritis may be painful and inflamed. Generally, the pain develops gradually over time, although sudden onset is also possible. There are other symptoms, as well:
- The joint may become stiff and swollen, making it difficult to bend and straighten the knee.
- Pain and swelling may be worse in the morning, or after sitting or resting.
- Vigorous activity may cause pain to flare up.
- Loose fragments of cartilage and other tissue can interfere with the smooth motion of joints. The knee may "lock" or "stick" during movement. It may creak, click, snap or make a grinding noise (crepitus).
- Pain may cause a feeling of weakness or buckling in the knee.
Many people with arthritis note increased joint pain with rainy weather.
Diagnosis
Physical Examination
During the physical examination, your doctor will look for:
- Joint swelling, warmth, or redness
- Tenderness about the knee
- Range of passive (assisted) and active (self-directed) motion
- Instability of the joint
- Crepitus (a grating sensation inside the joint) with movement
- Pain when weight is placed on the knee
- Problems with your gait (the way you walk)
- Any signs of injury to the muscles, tendons, and ligaments surrounding the knee
- Involvement of other joints (an indication of rheumatoid arthritis)
Imaging Tests
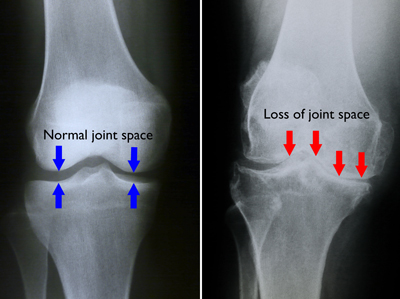
- X-rays. These imaging tests create detailed pictures of dense structures, like bone. They can help distinguish among various forms of arthritis. X-rays of an arthritic knee may show a narrowing of the joint space, changes in the bone and the formation of bone spurs (osteophytes).
Treatment
There is no cure for arthritis but there are a number of treatments that may help relieve the pain and disability it can cause.
Nonsurgical Treatment
As with other arthritic conditions, initial treatment of arthritis of the knee is nonsurgical. Your doctor may recommend a range of treatment options.
Lifestyle modifications. Some changes in your daily life can protect your knee joint and slow the progress of arthritis.
Minimize activities that aggravate the condition, such as climbing stairs.
Switching from high impact activities (like jogging or tennis) to lower impact activities (like swimming or cycling) will put less stress on your knee.
Losing weight can reduce stress on the knee joint, resulting in less pain and increased function.
Physical therapy. Specific exercises can help increase range of motion and flexibility, as well as help strengthen the muscles in your leg. Your doctor or a physical therapist can help develop an individualized exercise program that meets your needs and lifestyle.
Assistive devices. Using devices such as a cane, wearing shock-absorbing shoes or inserts, or wearing a brace or knee sleeve can be helpful. A brace assists with stability and function, and may be especially helpful if the arthritis is centered on one side of the knee. There are two types of braces that are often used for knee arthritis: An "unloader" brace shifts weight away from the affected portion of the knee, while a "support" brace helps support the entire knee load.
Other remedies. Applying heat or ice, using pain-relieving ointments or creams, or wearing elastic bandages to provide support to the knee may provide some relief from pain.
Medications. Several types of drugs are useful in treating arthritis of the knee. Because people respond differently to medications, your doctor will work closely with you to determine the medications and dosages that are safe and effective for you.
Injection therapy. PRP, Stem Cells, Corticosteroids, and Hyaluronic Acid may all be effective in treating knee arthritis
Surgical Treatment
Your doctor may recommend surgery if your pain from arthritis causes disability and is not relieved with nonsurgical treatment. As with all surgeries, there are some risks and possible complications with different knee procedures. Your doctor will discuss the possible complications with you before your operation.
Arthroscopic surgery is not often used to treat arthritis of the knee. In cases where osteoarthritis is accompanied by a degenerative meniscal tear, arthroscopic surgery may be recommended to treat the torn meniscus.
Knee replacement surgery is discussed when other treatment options have failed. This removes the arthritis from the knee and replaces the knee joint with a special implant. Some patients may meet criteria for a partial knee replacement. This is a less invasive option with a faster recovery.
Recovery
After any type of surgery for arthritis of the knee, there is a period of recovery. Most patients spend two nights in the hospital and then go home or to a rehab facility based on their individual needs.
After going home patients will participate in a supervised physical therapy program to maximize their strength and function in the knee.